Health
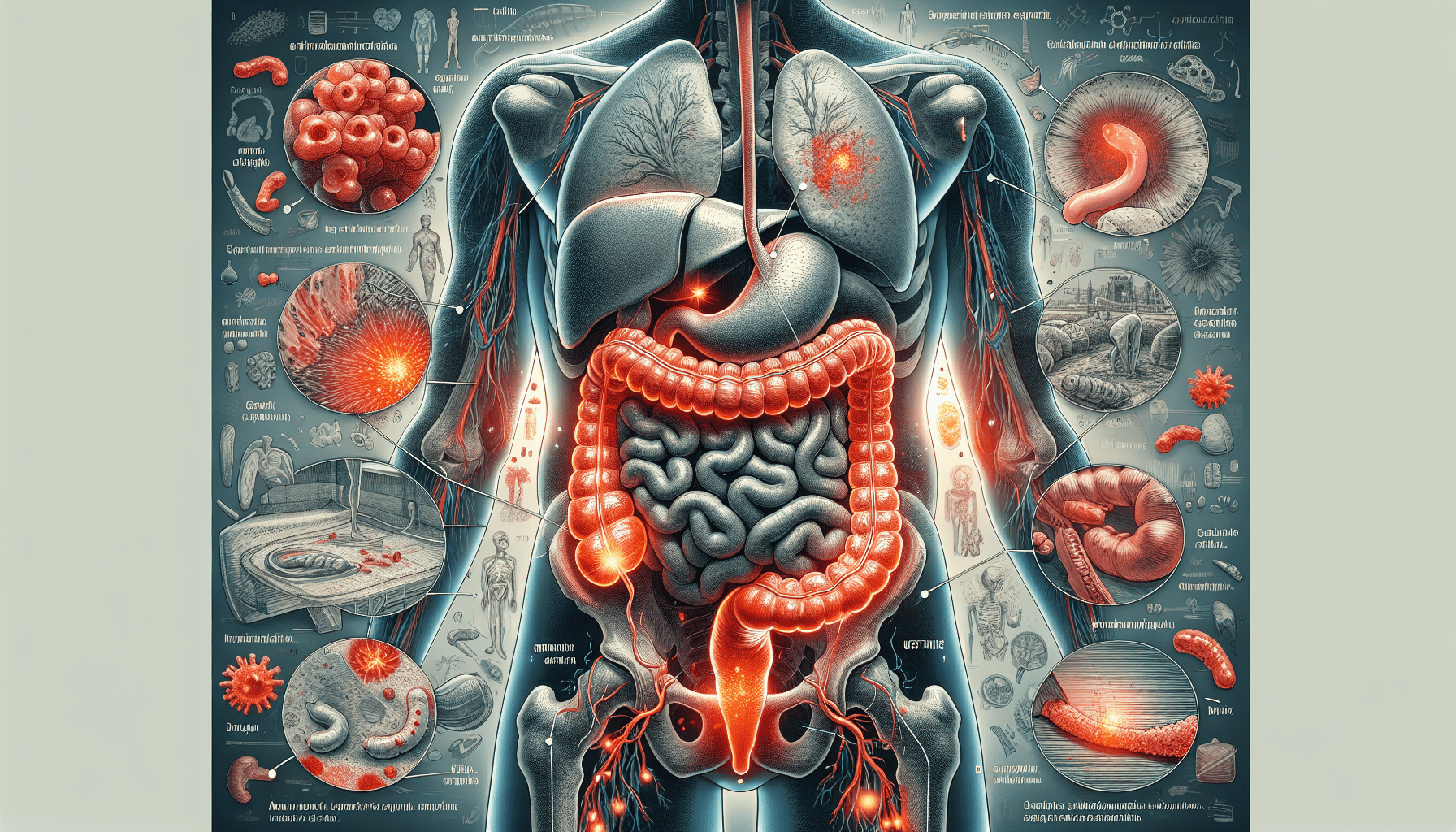
Understanding Inflammatory Bowel Disease
Gain a comprehensive understanding of Inflammatory Bowel Disease (IBD) in this informational post. Explore the types, causes, symptoms, diagnosis, treatment options, and complications of IBD to better manage this chronic condition. Let’s embark on this journey together.
In this article, you will gain a comprehensive understanding of Inflammatory Bowel Disease (IBD). This chronic condition affects millions of people worldwide, but with the right knowledge and support, managing its symptoms becomes more manageable. From exploring the different types of IBD to discussing the potential causes and common symptoms, this article aims to equip you with the necessary information to navigate this condition. So, let’s embark on this journey together and discover the ins and outs of Inflammatory Bowel Disease.
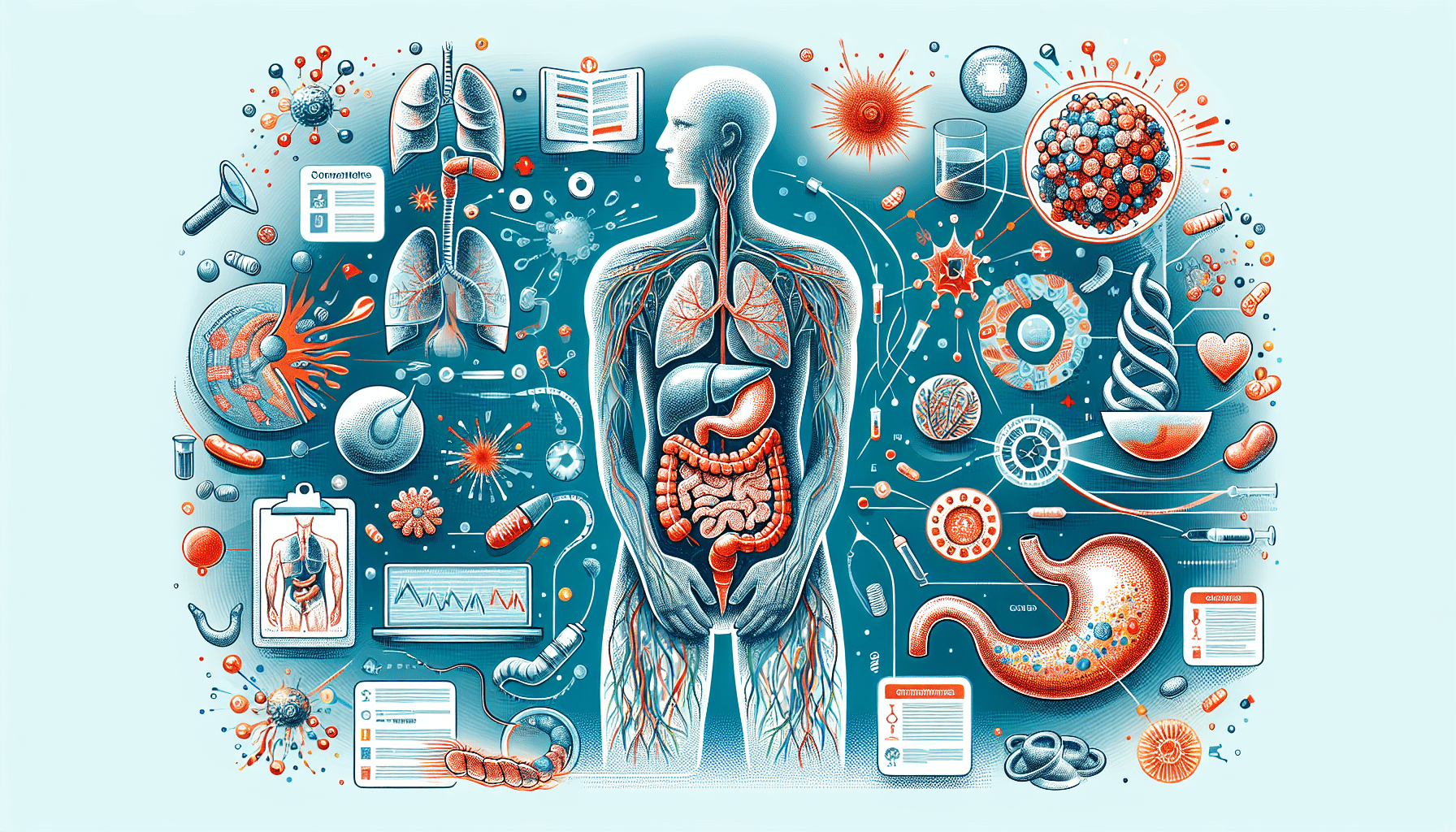
Definition of Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) is a chronic condition that affects the digestive tract, causing inflammation and damage. There are two main types of IBD: Crohn’s disease and ulcerative colitis.
Crohn’s Disease
Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus. It is characterized by inflammation that extends through the entire thickness of the bowel wall. This can lead to various symptoms and complications, such as abdominal pain, diarrhea, weight loss, and fatigue.
Ulcerative Colitis
Ulcerative colitis primarily affects the colon and the rectum. It involves inflammation and ulcers in the innermost lining of the large intestine. Symptoms of ulcerative colitis may include abdominal pain, rectal bleeding, diarrhea, and fever.
Causes and Risk Factors
The exact cause of inflammatory bowel disease is still unknown, but there are several factors that may contribute to its development.
Genetics
There is evidence to suggest that genetics plays a role in the development of IBD. If you have a family member with Crohn’s disease or ulcerative colitis, you may be at a higher risk of developing the condition yourself.
Environmental Factors
Environmental factors, such as diet, can also influence the development of IBD. Certain foods, such as high-fat or processed foods, may trigger flare-ups or worsen symptoms. Additionally, exposure to certain pollutants or infections may also play a role.
Immune System Dysfunction
It is believed that an abnormal immune response plays a significant role in triggering and perpetuating the inflammation seen in IBD. The immune system may mistakenly attack the healthy cells in the digestive tract, leading to chronic inflammation.

Signs and Symptoms
Inflammatory bowel disease can manifest with various signs and symptoms, which can vary in severity from person to person.
Abdominal Pain
Abdominal pain is a common symptom of inflammatory bowel disease. It is often described as cramping or a constant ache and is typically located in the lower right or lower left side of the abdomen.
Diarrhea
Frequent and loose bowel movements are another hallmark symptom of IBD. Diarrhea may be accompanied by urgency and a feeling of incomplete emptying of the bowels.
Rectal Bleeding
Rectal bleeding, often seen as bright red blood in the stool, is more commonly associated with ulcerative colitis. However, it can also occur in Crohn’s disease, particularly when the disease affects the rectum or anus.
Weight Loss
Unintentional weight loss is a common occurrence in individuals with inflammatory bowel disease. This is often due to the reduced absorption of nutrients from the inflamed intestines or decreased appetite caused by the disease itself.
Fatigue
Fatigue is a common complaint among those with IBD. The chronic inflammation and loss of nutrients can contribute to feelings of exhaustion and low energy levels.
Fever
Fever may occur during flare-ups of inflammatory bowel disease. It is often a sign of more severe inflammation and may be accompanied by other systemic symptoms.
Diagnosis
To accurately diagnose inflammatory bowel disease, your healthcare provider will typically employ a combination of medical history, physical examination, and various tests.
Medical History and Physical Examination
Your healthcare provider will start by taking a detailed medical history, including any symptoms you may be experiencing. They will also perform a physical examination to assess your overall health and check for signs of inflammation, such as tenderness in the abdomen.
Blood Tests
Blood tests can help identify markers of inflammation in the body, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). These tests can help confirm the presence of inflammation and determine the overall severity of the disease.
Stool Tests
Stool tests may be performed to check for the presence of blood, infectious agents, or other abnormalities. These tests can help differentiate between inflammatory bowel disease and other conditions that may cause similar symptoms.
Colonoscopy
A colonoscopy is a procedure that allows a visual examination of the colon and the rectum. During a colonoscopy, your healthcare provider will insert a thin, flexible tube with a camera into your anus to examine the lining of your digestive tract for abnormalities.
Biopsy
During a colonoscopy, your healthcare provider may take small tissue samples, known as biopsies, from the inflamed areas. These samples are then examined under a microscope to confirm the diagnosis and determine the type and severity of the disease.
Types of Inflammatory Bowel Disease
Inflammatory bowel disease encompasses several different conditions, with Crohn’s disease and ulcerative colitis being the most common.
Crohn’s Disease
Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus. It can cause inflammation and damage in any segment of the gastrointestinal tract, resulting in a variety of symptoms and complications.
Ulcerative Colitis
Ulcerative colitis primarily affects the colon and the rectum. It causes inflammation and ulcers in the innermost lining of the large intestine, leading to symptoms such as abdominal pain, rectal bleeding, and diarrhea.
Indeterminate Colitis
In some cases, it may be challenging to definitively diagnose whether a patient has Crohn’s disease or ulcerative colitis. When the characteristics of the disease do not clearly meet the criteria for either condition, it is referred to as indeterminate colitis.
Treatment Options
The goal of treatment for inflammatory bowel disease is to reduce inflammation, relieve symptoms, and achieve and maintain remission. The treatment approach will vary depending on the severity and type of IBD.
Medication
Medication is a cornerstone of treatment for inflammatory bowel disease. There are various types of drugs used to manage symptoms and reduce inflammation, including anti-inflammatory drugs, immunomodulators, biologic therapies, and corticosteroids.
Lifestyle Changes
In addition to medication, certain lifestyle changes can help manage inflammatory bowel disease and improve overall well-being. These may include dietary modifications, stress management techniques, regular exercise, and smoking cessation.
Surgery
In some cases, surgery may be necessary to manage complications or to remove the affected portion of the digestive tract. Surgery can provide relief and improve quality of life for those with severe or refractory inflammatory bowel disease.

Medication for Inflammatory Bowel Disease
Medication plays a crucial role in the management of inflammatory bowel disease. Different types of medication are used to target the underlying inflammation and alleviate symptoms.
Anti-inflammatory Drugs
Anti-inflammatory drugs, such as aminosalicylates and corticosteroids, help reduce inflammation in the digestive tract. They can help alleviate symptoms and induce remission in mild to moderate cases of IBD.
Immunomodulators
Immunomodulators, such as thiopurines and methotrexate, work by suppressing the immune system to reduce inflammation. These medications are often used to maintain remission and prevent flare-ups in individuals with moderate to severe IBD.
Biologic Therapies
Biologic therapies target specific proteins or cells in the immune system that contribute to inflammation. Medications such as anti-TNF agents (e.g., infliximab) and integrin inhibitors (e.g., vedolizumab) are examples of biologic therapies used to manage moderate to severe inflammatory bowel disease.
Corticosteroids
Corticosteroids, such as prednisone, are potent anti-inflammatory medications that can provide short-term relief for individuals with severe flares of inflammatory bowel disease. However, their use is typically limited due to potential side effects when used long term.
Lifestyle Changes to Manage Inflammatory Bowel Disease
In addition to medication, certain lifestyle changes can help individuals with inflammatory bowel disease better manage their symptoms and improve overall well-being.
Dietary Modifications
Making dietary modifications can be beneficial in managing inflammatory bowel disease. Some individuals may find that avoiding trigger foods, such as spicy or high-fiber foods, can help reduce symptoms. Others may benefit from maintaining a well-balanced diet that ensures adequate nutrient intake.
Stress Management
Stress has been shown to aggravate symptoms of inflammatory bowel disease. Implementing stress management techniques, such as mindfulness, yoga, or deep breathing exercises, can help reduce stress levels and improve overall well-being.
Regular Exercise
Regular physical activity has numerous benefits for individuals with inflammatory bowel disease. Exercise can help reduce inflammation, improve mood, boost energy levels, and maintain overall physical fitness. However, it is important to consult with your healthcare provider before starting a new exercise regimen.
Smoking Cessation
Smoking has been linked to an increased risk and severity of inflammatory bowel disease. Quitting smoking can significantly improve outcomes and reduce the risk of complications. If you smoke and have inflammatory bowel disease, it is important to discuss smoking cessation strategies with your healthcare provider.
Complications of Inflammatory Bowel Disease
Inflammatory bowel disease can lead to various complications that may require additional treatment or management.
Intestinal Obstruction
Inflammation and scarring of the digestive tract can cause partial or complete blockages, leading to intestinal obstructions. These obstructions can cause severe abdominal pain, bloating, and vomiting and may require hospitalization and surgical intervention.
Abscesses
Inflammatory bowel disease can lead to the formation of abscesses, which are pockets of pus that develop as a result of infection. Abscesses typically cause localized pain, swelling, and fever and may require drainage through a medical procedure.
Fistulas
Fistulas are abnormal connections between different parts of the digestive tract or between the digestive tract and other organs. They can develop as a result of ongoing inflammation in inflammatory bowel disease. Fistulas may lead to complications such as infections and require surgical intervention.
Malnutrition
Inflammatory bowel disease can interfere with the body’s ability to absorb nutrients from food, leading to malnutrition. Proper nutrition and working with a registered dietitian can help prevent malnutrition and ensure adequate nutrient intake.
Colon Cancer
Long-term inflammation of the colon in ulcerative colitis can increase the risk of developing colon cancer. Regular monitoring and surveillance through regular colonoscopies are crucial in detecting any precancerous changes and ensuring early intervention if necessary.
Living with Inflammatory Bowel Disease
Living with inflammatory bowel disease can present challenges, but with the right support and self-care strategies, it is possible to lead a fulfilling life.
Emotional Support
Seeking emotional support from loved ones, support groups, or mental health professionals can be beneficial. Living with a chronic condition like inflammatory bowel disease can be emotionally challenging, and having a support system in place can help alleviate stress and improve overall well-being.
Self-care Strategies
Taking care of yourself is essential when living with inflammatory bowel disease. This may involve practicing good hygiene, getting enough rest, and managing stress levels. It is also important to adhere to your prescribed treatment plan and attend regular medical appointments.
Managing Flares
Flares, or periods of increased disease activity, can occur in individuals with inflammatory bowel disease. It is important to recognize the signs of a flare and have a plan in place to manage symptoms. This may involve adjusting medication, following a specific diet, or contacting your healthcare provider for further guidance.
In conclusion, inflammatory bowel disease is a chronic condition that can significantly impact the lives of those affected. Understanding the causes, symptoms, diagnosis, and treatment options are crucial for managing the disease effectively. With a combination of medication, lifestyle changes, and emotional support, individuals with inflammatory bowel disease can lead fulfilling lives and minimize the impact of the disease on their overall well-being.